Periodontal Assessment
Periodontal Assessments in Arlington Heights and Mount Prospect, IL
Periodontal assessment is an essential part of each hygiene appointment. We determine periodontal status of our patients by assessing loss of attachment (probing depths, recession, MGI), bleeding, furcation involvement, teeth mobility, bone level and gum appearance.

Probing Depths
Probe depths are part of comprehensive periodontal assessment and are used to obtain information about health status of the periodontium. Hygienist measures distance from the gingival margin to junctional epithelium (base of the pocket). Normal healthy pocket measures 1-3 mm. When there is an apical migration of the junctional epithelium the tissue becomes diseased and the reading is ≥ 4 mm. Teeth with moderate to severe probing depths are at higher risk of bone loss.

Most of the time increasing pockets depths indicate gum disease caused by the body’s immune response to bacteria and tartar deposit which is attached to the teeth. Thorough cleaning and patient’s role with self-care would help to stop the damaging action of harmful bacteria and thus prevent progressing of periodontal disease.

Recession
Recession is a migration of free gingiva towards the root apex, resulting in exposure of the root surface. Presence of recession indicates attachment loss.
The etiology of recession can come from many different factors. It can be caused due to:
- periodontal disease (presence of periodontal pocket, bone loss)
- mechanical trauma (hard toothbrush, hard pressure when brushing teeth, parafunctional habits such as grinding, clenching or heavy bite)
Recession can contribute to tooth hypersensitivity, root caries, or an unpleasant esthetic appearance.
When there is plaque and calculus present, which consists of a large amount of harmful bacteria, the body’s immune response tries to fight it off and along run destroys the surrounding bone and tissue. Due to this process bone loss progresses so does the gum is moving down with it.

Bleeding
Bleeding is an early sign of tissue inflammation and can be a useful measurable diagnostic tool. Healthy gingiva doesn’t bleed spontaneously, when patient brushes, flosses or when hygienist performs probing.
If bleeding appears it indicates gum infection that mainly might be caused by bacteria and deposit accumulation (plaque or tartar) around teeth and below gumline. Bacteria make the gums red, tender, swollen and bleed easily. This gum infection is called GINGIVITIS.
If gingival inflammation progresses into deeper periodontal structures it leads to damage of the bone that holds the teeth in place. Then we talk about PERIODONTITIS – serious bacterial infection.
We re-check pockets and bleeding at each appointment. If after periodontal treatment patient still bleeds in some places it means that there is still inflammation and additional treatment of these areas is needed. If the bleeding significantly decreased it indicates that the treatment was successful and patient self-care has improved.
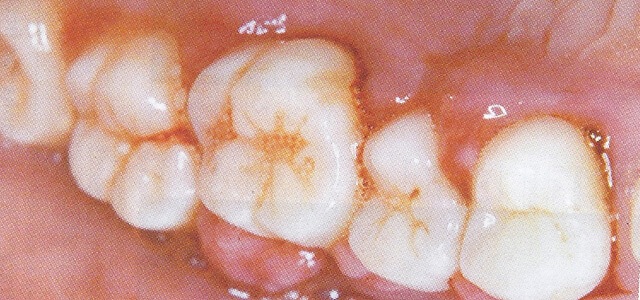

Furcation Involvement
Furcation is a separation between the roots of multirooted teeth. Furcation involvement means that the space between roots is exposed due to bone destruction and loss of attachment.
Furcations harbor plaque and bacteria easier than healthy teeth. We give a thorough explanation of the importance of proper self-care in these areas.

Use floss threader to clean furcation space

MGI
There is a band of gum that surrounds teeth that is hard and is attached to the bone. It is called attached gingiva. This tissue helps protect the teeth from mechanical forces such as eating and brushing. This band of gum is in a healthy state when it is 1+ mm of width.
Mucogingival involvement (MGI) is when there is no remaining attached gingiva. This means that the tooth is losing stability, and has the chance of becoming more mobile which could lead to a hopeless prognosis.
MGI can come from the complete loss of attachment due to multiple factors such as deep probe depths, recession, bone loss, furcation involvement, and periodontal abscess.

Healthy attached gingiva. Arrows shows pale pink, firm and dense attached gingiva tightly connected to the root and bone. Dashed line indicates the junction between attached gingiva and alveoral mucosa which is dark red color surface.

Photo shows MGI due to recession. Arrows indicate exposed roots and lack of attached gingiva on a tooth surface. Involved teeth are surrounded just by a dark red and thin alveolar mucosa.

Mobility
Mobility is a movement of the tooth and may be a clinical sign of attachment loss, occlusal trauma, inflammation or diseases of the jaw. In general all teeth are slightly mobile due to a nature of the periodontal ligament which attaches tooth to the bone.
We check for mobility to see how stable the teeth are in the mouth and if it has progressed since last hygiene appointment.

Left: Healthy bone level – teeth stable Right: Teeth affected by a periodontal disease and severe bone loss are significantly more mobile.
Get Professional Dental Treatment Today
To determine periodontal health we also evaluate patient’s radiographs. We check for bone level, tartar deposit under gumline, periodontal ligament space, presence of dental decay, faulty restoration, furcation involvement, open contacts etc. When it’s time for treatment by a dental professional, give us a call and schedule an appointment. Reach out to our office by calling 847-758-0100 at your earliest convenience!
